DIABETIC RETINOPATHY
The cells in persons with diabetes mellitus have difficulty using and storing sugar properly. When blood sugar gets too high, it can damage the blood vessels in the eyes. This damage may lead to diabetic retinopathy.
The two types of diabetic retinopathy are Proliferative diabetic retinopathy and Non Proliferative diabetic retinopathy.
PROLIFERATIVE DIABETIC RETINOPATHY
New, fragile blood vessels grow on the surface of the retina. These new blood vessels are called neovascularization, and can lead to serious vision problems, because the new vessels can break and bleed into the vitreous. When the vitreous becomes clouded with blood, light is prevented from passing through the eye to the retina.
Types : The two common types of macular degeneration are "dry" and "wet."
This can blur or distort vision and frequently causes sudden and severe loss of vision. The new blood vessels can also cause scar tissue to develop, which can pull the retina away from the back of the eye. This is known as retinal detachment, and can lead to blindness if untreated. In addition, abnormal blood vessels can grow on the iris (the colored part in the front of the eye), which can lead to severe glaucoma.
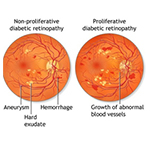
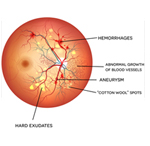
Background or nonproliferative diabetic retinopathy - blood vessels in the retina are damaged and can leak fluid or bleed. This causes the retina to swell and form deposits called exudates.
Many patients may not notice any change in their vision when they develop this early form of the disease, but it can lead to other more serious forms of retinopathy that severely affect vision. Fluid collecting in the macula is called macular edema and may cause difficulty with reading and other close work.
TREATMENT OF DIABETIC RETINOPATHY :
Good control of diabetes with intensive management and control of blood sugar will delay, and possibly prevent, both the development and progression of diabetic retinopathy. Patients with diabetic retinopathy frequently need to have special photographs of the retina taken. This series of photos is called fluorescein angiography.
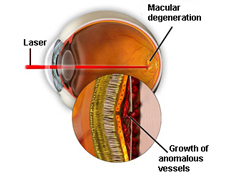
Laser photocoagulation is one of the most common treatments for diabetic retinopathy. Focal photocoagulation consists of laser directed at the retina to seal leaking blood vessels in patients with background diabetic retinopathy. Panretinal photocoagulation consists of laser spots scattered through the sides of the retina to reduce abnormal blood vessel growth (neovascularization) and help seal the retina to the back of the eye in patients with proliferative diabetic retinopathy. This can help prevent retinal detachment. There is little recuperation needed after laser surgery for diabetic retinopathy. Laser surgery may require more than one treatment to be effective.
Vitrectomy surgery is performed for patients with very advanced proliferative diabetic retinopathy or retinal detachment. In vitrectomy, the surgeon removes the blood-filled vitreous and replaces it with a clear solution. This allows light to pass through the clear fluid to the retina, where the images are conveyed to the brain.
Pharmacotherapy : Increasingly, a variety of medications are being used to treat the manifestations of background and proliferative diabetic retinopathy.
These involve intravitreal injections of small amounts of medication into the eye.
The type of retinopathy, as well as the patient's general health and eye structure will determine the kind of treatment needed and the type of anesthesia utilized.