Understanding Keratoconus - Corneal Changes, Causes, and Treatment
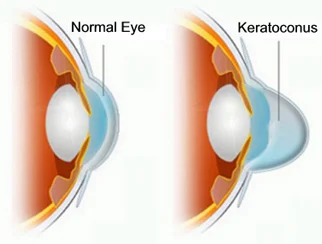
Keratoconus is a progressive eye disease that causes the normally round cornea to thin and gradually bulge into a cone shape. This change in shape alters how light enters the eye, leading to distorted and blurry vision as it reaches the retina.
This condition is non-inflammatory, meaning it doesn’t involve swelling or redness, but it is a long-term issue that can worsen over time. As the cornea becomes thinner and steeper, the patient may experience a significant loss of vision, which can range from mild to severe depending on how much the cornea is affected.
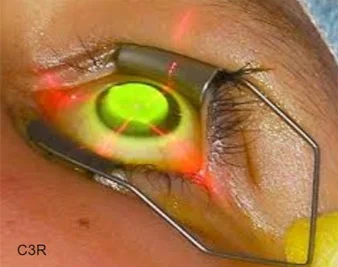
The latest revolutionary Keratoconus treatment is C3R (Corneal Collagen Crosslinking with Riboflavin) that has been proven to strengthen the weak corneal structure & by increasing collagen crosslinking, which are the natural “anchors” within the cornea. These anchors are responsible for preventing the cornea from bulging out and becoming steep and irregular, consequence of advanced Keratoconus.
Early Stages – Spectacles and Contact Lenses
In the early stages, vision can often be corrected with glasses, which help to focus light more accurately on the retina. However, as keratoconus progresses and the cornea becomes more irregular, glasses may no longer be effective, and rigid contact lenses become necessary. These lenses provide a smoother, more regular refracting surface, improving vision. However, regular use can sometimes cause corneal scarring, so patients should be made aware of this possibility.
Advanced Treatment – C3R (Corneal Collagen Crosslinking with Riboflavin)
For advanced cases, the latest treatment option is C3R - Corneal Collagen Crosslinking with Riboflavin. This innovative procedure strengthens the cornea by increasing the natural crosslinks in the corneal tissue, acting like internal "anchors" to prevent further thinning and bulging. This approach can stabilize the cornea, reduce the need for more invasive surgeries, and improve long-term vision stability.
Consulting a keratoconus specialist in Mumbai can help you understand your condition better and select the most suitable treatment plan. Our experts provide personalized care and access to the latest treatment options, ensuring the best possible vision outcomes.
Causes of Keratoconus
Keratoconus is a complex corneal condition, and while the exact cause remains unclear, several factors are believed to increase the risk:
Genetic Influence - Keratoconus often runs in families, suggesting a genetic link. If a parent or sibling has keratoconus, the likelihood of developing the condition is higher.
Eye Rubbing - Frequent or aggressive eye rubbing has been linked to keratoconus, as it can weaken the cornea over time. This is particularly common in people with allergies or chronic eye irritation.
Underlying Medical Conditions - Certain medical conditions, like asthma, Down syndrome, Ehlers-Danlos syndrome, and other connective tissue disorders, are associated with a higher risk of developing keratoconus.
Environmental Factors - Exposure to UV rays, eye allergies, and long-term eye irritation may also contribute to the weakening of the cornea, potentially leading to keratoconus.
Hormonal Changes - Some studies suggest that hormonal fluctuations during puberty and pregnancy might influence the onset or progression of keratoconus.
Advanced keratoconus treatment in Mumbai at Kenia Eye Hospital includes procedures like C3R which can slow down the disease progression.
Symptoms of Keratoconus
Keratoconus can significantly impact your vision, often starting with subtle changes that become more noticeable over time. Recognizing the early signs can help ensure timely diagnosis and treatment.
- Frequent Prescription Changes: If you find yourself needing to update your glasses or contact lens prescriptions more often than usual, it could be a sign of keratoconus.
- Blurry and Distorted Vision: As the cornea thins and changes shape, it can cause blurry, distorted, or double vision.
- Light Sensitivity and Glare: Many patients with keratoconus experience increased sensitivity to light, along with halos or glare, especially at night.
- Eye Irritation: Some people may notice discomfort, dryness, or a gritty sensation in their eyes.
- Corneal Scarring: In advanced cases, the cornea can develop scars, leading to further vision loss and the potential need for a corneal transplant.
If you notice these symptoms and are considering keratoconus treatment in Mumbai, we can help you explore effective options to preserve your vision and improve your quality of life.
Keratoconus Treatment
Early detection is essential for managing keratoconus effectively. Diagnosing the condition in its early stages allows for better control over its progression and can help prevent severe vision loss.
Early Detection and Diagnosis
Keratoconus is typically diagnosed through a series of specialized eye tests, including:
- Retinoscopy: A simple test to check how light reflects from the retina.
- Slit Lamp Examination: A detailed assessment of the front structures of the eye, including the cornea.
- Topography and Pentacam Scans: These advanced imaging tests measure the curvature and shape of the cornea, providing a precise map of its surface.
- Pachymetry: This test measures the thickness of the cornea, which is critical for detecting early thinning.
In the advanced stages of keratoconus, standard glasses often fail to correct vision effectively, and patients may need hard or semi-soft contact lenses. These lenses help create a smoother refracting surface, improving vision. However, a proper fit is crucial, as poorly fitting lenses can cause discomfort, corneal abrasions, scarring, or even infections.
Treatment Options
- Glasses and Contact Lenses: In the early stages, specially designed lenses can help improve vision by providing a more regular surface over the irregular cornea.
- Corneal Collagen Cross-Linking (C3R): This advanced procedure strengthens the cornea by increasing the natural collagen cross-links, which helps stabilize the cornea and prevent further progression.
- Corneal Strengthening – Collagen Cross-Linking (C3R) with Riboflavin - It is a non-invasive treatment for keratoconus. It works by strengthening the collagen fibers that form the structure of the cornea, helping to stabilize its shape and prevent further thinning.
This in-office procedure typically takes about 60 minutes. During the treatment, riboflavin (Vitamin B2) eye drops are applied to the cornea, which is then exposed to controlled ultraviolet (UV) light. This combination triggers the cross-linking process, increasing the strength of the corneal tissue by up to 300%, reducing the risk of further bulging and slowing the progression of keratoconus.
In more severe cases, C3R can be combined with Intacs, which are small, crescent-shaped plastic rings placed within the cornea. These rings help flatten the cone shape, improving vision by making the cornea more regular, while the C3R treatment strengthens the overall structure to prevent further progression.
This approach can be highly effective in stabilizing the condition, reducing the need for more invasive procedures like corneal transplants.
- INTACS: These are tiny implants that can be placed in the cornea to flatten its shape and improve vision, reducing the need for corneal transplant surgery.
Keratoplasty (Corneal Transplantation) :
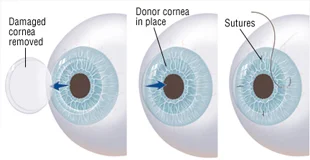
When other treatments for keratoconus are no longer effective in restoring clear vision, a corneal transplant, known as keratoplasty, may be necessary. This procedure involves replacing the damaged cornea with a healthy donor cornea, helping to restore the eye’s natural shape and improve vision.
In advanced cases where the cornea has become too thin or scarred, a transplant is often the only option for restoring useful vision.
What to Expect with Keratoplasty:
- It is an intraocular surgery, meaning it involves the inside of the eye.
- Recovery can take several months, and patients need long-term follow-up to monitor healing and prevent complications.
- The success of the surgery depends on proper care, regular check-ups, and a commitment to following your eye specialist’s advice.
Access to keratoconus treatment near me means you can get timely care and personalized treatment. Choose Kenia Eye Hospital where we offer advanced diagnostic tools and the latest treatment options to help manage keratoconus effectively and preserve your vision.
FAQs
Squint
What is keratoconus, and how does it affect vision?
Keratoconus is a condition where the cornea, the clear front part of the eye, becomes thin and starts to bulge into a cone shape. This irregular shape distorts light entering the eye, leading to blurry and distorted vision.
What are the common signs of keratoconus?
Early signs include frequent changes in glasses or contact lens prescriptions, blurry or double vision, increased sensitivity to light, and halos around lights at night. In advanced stages, the cornea may become scarred, causing further vision loss.
How is keratoconus diagnosed?
Keratoconus is usually diagnosed through a detailed eye exam, which may include tests like corneal topography, pachymetry, and slit-lamp examination to check the thickness and shape of the cornea.
Can keratoconus be treated without surgery?
Yes, in the early stages, vision can often be managed with glasses or specially designed contact lenses. More advanced cases may require treatments like Corneal Collagen Cross-Linking (C3R) to strengthen the cornea and slow progression.
When is a corneal transplant needed for keratoconus?
A corneal transplant is usually considered when other treatments no longer provide clear vision, or if the cornea becomes too thin or scarred to support a contact lens.